- Solutions
- Solutions
- Home Health
- Hospice
- Life Plan Community
- Palliative Care
- Private Duty
- Senior Living
- Skilled Nursing
- Skilled Nursing
- Skilled Nursing Software
- Advanced Insights
- Customer relationship management
- Data and analytics
- Financial & operations management
- Marketing
- Nutrition management
- Referral management
- Regulatory compliance
- Retail management
- Resident engagement
- Revenue cycle management
- Skilled nursing interoperability
- Partners
- Blogs
- Resources
- About
- User Conference

5 Benefits of documenting at the point of care
With a staffing shortage that continues to rise across post-acute care and constantly evolving regulations, including the expansion of the Home Health Value-Based Purchasing Model, having technology that allows clinicians to document at the point of care can ease their administrative burden and help to improve the patient experience.
Here are five benefits of documenting at the point of care:
1. It can improve work-life balance.
A common challenge for clinicians is not being able to complete their documentation during their workday. This forces them to finish their work when they are home with their families in the evening. When documentation is completed at the point of care, clinicians can de-stress and fully enjoy non-interrupted time with their families after work hours. It also helps to eliminate duplicate work such as handwriting a note during a visit, only to re-enter the same information into the EMR later in the day.
When the clinician completes their visit note documentation at home later in the day, they may find there are additional questions or areas that require re-assessment that can no longer be assessed due to a delay in the documentation; additional follow-up with the patient and/or family will then be required. This causes additional work and increased stress for the clinician. Completing documentation at the point of care results in a less stressful working environment and increased staff satisfaction because clinicians can truly enjoy their time off.
2. It can improve documentation accuracy and quality of care.
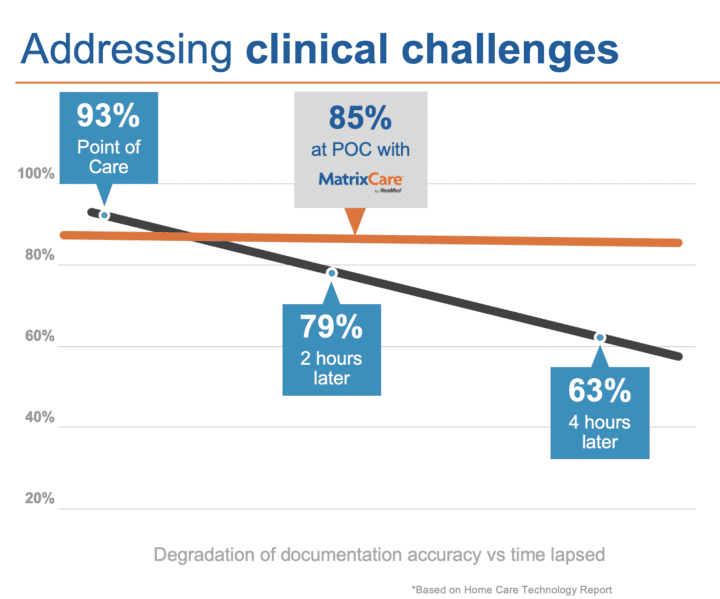
When handwritten notes taken during the visit need to be entered into the EMR later in the day, accuracy can be greatly decreased. In fact, based on the Homecare Technology Report, clinicians have been shown to only document at 63% accuracy when the documentation is completed four hours following the visit.
In addition, loose paper notes are not secure and are at risk of being lost and/or viewed by someone other than the clinician.
Point-of-care documentation also allows clinicians to reassess the plan of care and make immediate changes as needed when they are in the patient’s home. It’s a proactive approach that decreases the probability of errors and increases quality of patient care, ultimately increasing efficiency of documentation and allowing clinicians the bandwidth to focus more on patients.
3. It can improve safety.
Documentation at the point of care allows the clinician to address any alerts or interactions in real time. For example, medications reviewed or added during medication reconciliation may trigger interaction alerts that can be addressed immediately while in the patient home. In addition, documenting in real time allows office, on-call, and triage staff to have the most up-to-date data on the patient at any given time, which is crucial to providing the best possible care.
Documenting at the bedside also promotes continued education with the patient and caregiver regarding their current plan of care, active medication list, etc. And it provides the ability to make changes as needed while in the home to prevent any delays.
4. It can improve productivity.
Using an EHR with built-in workflows and logic streamlines the documentation, allowing staff to complete more visits while still prioritizing quality and safety. Empowering clinicians to do more with less increases job satisfaction and patient and family engagement — a win-win for everyone involved in the care journey.
5. It can improve billing and reimbursement.
Every agency is going to experience a billing or claim rejection, but the right technology can help avoid cash flow problems. Due to documentation at the point of care helping to increase accuracy and efficiency, billing and claims holds from outstanding visits will decrease while increasing timely reimbursement.
Consider an EHR that helps to enhance efficiencies for your current staff
Stress less on finding new talent, and instead focus on your current staff by considering an EHR with these capabilities:
- Medication import allows clinicians to spend more time with the patient, as imported medications don’t need to be manually entered prior to medication reconciliation.
- The ability to document disconnected allows clinicians to document at the bedside, even if in remote areas.
- Logic built into assessments streamlines documentation for the clinicians and improves quality while also increasing their ability to complete visits while at the point of care.
- Integrated speech-to-text improves the quality of notes and increases staff satisfaction, as they can document timely at the point of care.
- Electronic forms allow clinicians to have the patient and/or caregiver sign the form or document easily on the device at the bedside. This decreases the need for paper, and allows for better routing and tracking
It’s about more than documenting — it’s about improving the patient experience and giving staff the work-life balance they deserve.
Request a demo to see MatrixCare’s unique approach to documentation at the point of care.
See what MatrixCare can do for you
Carey Schmidt
As an RN and Solutions Consultant Manager for Matrixcare, Carey has spent the last six years in implementation as well as in her current role. She has 30 years of nursing experience, with 14 of those years specific to the post -acute space for both home health and hospice in the field as a clinician. She has also held leadership roles in inpatient case management, private duty, and home health, hospice, and palliative care. In addition to her nursing degree, Carey also has a bachelor’s degree in Healthcare Management – Informatics.
Related Posts


See MatrixCare in action
Start by having a call with one of our experts to see our platform in action.
MatrixCare offers industry-leading software solutions. Thousands of facility-based and home-based care organizations trust us to help them improve efficiency and provide exceptional care.




