- Solutions
- Solutions
- Home Health
- Hospice
- Life Plan Community
- Palliative Care
- Private Duty
- Senior Living
- Skilled Nursing
- Skilled Nursing
- Skilled Nursing Software
- Advanced Insights
- Customer relationship management
- Data and analytics
- Financial & operations management
- Marketing
- Nutrition management
- Referral management
- Regulatory compliance
- Retail management
- Resident engagement
- Revenue cycle management
- Skilled nursing interoperability
- Partners
- Blogs
- Resources
- About
- User Conference

Get ready to compete on performance: Understanding the expanded HHVBP Model measures
The original Home Health Value-Based Purchasing (HHVBP) Model was finalized in the calendar year (CY) 2016 HH final rule and implemented from January 1, 2016, through December 31, 2021, by the CMS Center for Medicare and Medicaid Innovation. Originally implemented in nine states (MA, MD, NC, FL, WA, AZ, IA, NE, TN), all Medicare-certified home health agencies (HHAs) in those nine states competed on value where payment was tied to quality performance—with payments adjusted upward or downward from a maximum adjustment of 3% in 2016, to a maximum adjustment of 7% in 2021.
This model has been very successful, resulting on average a 4.6% improvement in HHA performance and an annual savings to Medicare of about $141 million. Model assessment findings also demonstrated reductions in unplanned acute care hospitalizations and skilled nursing facility stays, which promoted the determination by the U.S. Secretary of Health and Human Services (HHS) that the expansion of the original HHVBP model would continue to reduce Medicare spending and improve the quality of care.
On January 8, 2021, CMS announced its intent to expand the HHVBP Model nationwide. Subsequently, on November 2, 2021, CMS published the CY 2022 home health final rule establishing the end of the original model and the start of the expanded model. This final rule also established HHA eligibility criteria, payment adjustment rates, definition of cohorts, applicable quality measures, and payment methodology.
<p> words
How can HHAs prepare to compete on performance?
The expanded HHVBP Model began on January 1, 2022, with CY 2022 being the pre-implementation year, and includes Medicare-certified HHAs in all 50 states, District of Columbia, and the U.S. territories.
During 2022, CMS is providing HHAs with resources and training to allow agencies time to prepare and learn about the expectations and requirements of the expanded HHVBP Model without risk to payments. The first full performance year for the expanded HHVBP Model is CY 2023, beginning January 1, 2023. CY 2025 will be the first payment year, with payment adjustment amounts upward or downward of 5%, which will be determined on CY 2023 performance.
In the expanded model, “cohorts” are determined based on each HHA’s unique HHCAHPS survey-eligible beneficiary count in the calendar year prior to the performance year. HHAs are assigned to either a nationwide larger-volume cohort or nationwide smaller-volume cohort. This approach groups HHAs that are of similar size and are more likely to receive scores on the same set of measures for purposes of setting benchmarks and achievement thresholds and determining payment adjustments.
Data from OASIS, HHCAHPS, and claims-based measures are used to calculate HHAs’ Total Performance Score in a performance year, which is a numeric score awarded to each HHA based on the weighted sum of the performance scores for each applicable measure.
What are the expanded HHVBP Model measures?
In selecting the applicable measures for inclusion in the expanded HHVBP Model, CMS has applied principles from the CMS Meaningful Measures Initiative, and considered the domains of the CMS Quality Strategy that map to six National Quality Strategy (NQS) priority areas:
- Make care safer by reducing harm caused in the delivery of care
- Strengthen person and family engagement as partners in their care
- Promote effective communication and coordination of care
- Promote effective prevention and treatment of chronic disease
- Work with communities to promote best practices of healthy living
- Make care affordable
HHAs will be evaluated using measures designed to include multiple (NQS) domains, in addition to providing future flexibility to incorporate and study newly developed measures over time. There are three data sources for the expanded HHVBP Model quality measures: OASIS-based data, Medicare fee-for-service claims data, and HHCAHPS survey-based data.
The payment adjustments for the expanded HHVBP Model apply only to home health PPS claims for Medicare fee-for-service (FFS) beneficiaries. However, the OASIS-based quality measures and HHCAHPS survey-based measures used in the model are calculated using data from all Medicare and Medicaid payors (Medicare FFS, Medicare Advantage, Medicaid FFS, Medicaid Managed Care). While the data from these measures comes from patients with all Medicare and Medicaid payors, an HHA’s payment adjustment will be applied only to Medicare home health FFS claims for Medicare FFS beneficiaries.
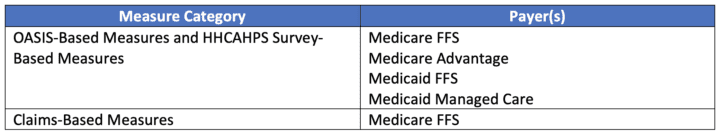
Source: https://innovation.cms.gov/media/document/hhvbp-exp-model-guide
Of the 12 currently approved quality measures to be used in the expanded HHVBP Model, there are five OASIS-based measures, two Medicare FFS claims-based measures, and five HHCAHPS survey-based measures. All measures in the expanded model use data already submitted by HHAs to meet the requirements of the Home Health Quality Reporting Program (HHQRP) and the submission of claims, therefore there is no need for agencies to submit additional data to fulfill the requirements of the expanded model. Also, most of the current expanded HHVBP measures cross several CMS quality improvement initiatives, so it is important for HHAs to develop an understanding of the source and use of each measure.
The table below provides an overview of the current approved expanded HHVBP model measures, their data sources, applicable CMS quality improvement initiatives, and links to the measure specifications.
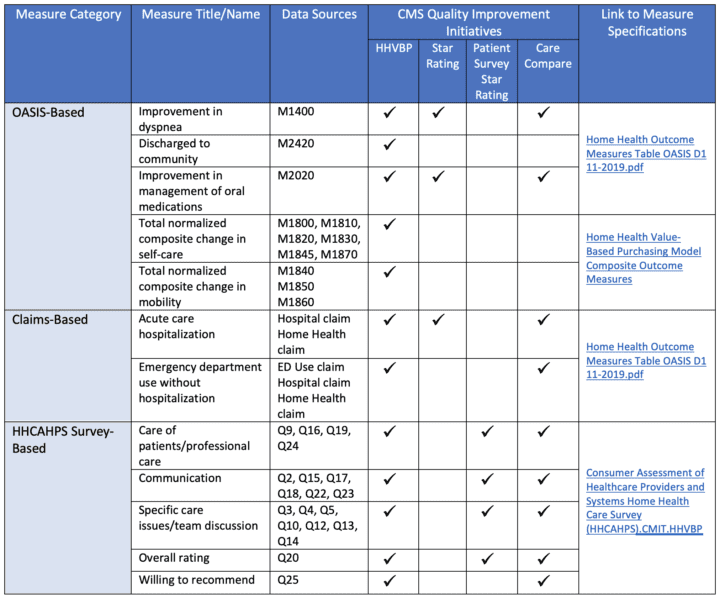
Source: https://innovation.cms.gov/media/document/hhvbp-exp-qm-webinar-slides
The HHAs that will be best positioned for success with the expanded HHVBP Model performance will be those that understand the model measures and are realigning their current Quality Assessment and Performance Improvement (QAPI) programs to focus on their identified skills gaps and areas of opportunity to improve clinical competence with OASIS assessments, focus on patient satisfaction, and continue to reduce hospitalization and urgent care utilization.
As we all know, data analysis is critical for preparing for the HHVBP Model and your software platform and analytics will play a critical role in your success. Don’t be behind when the CY 2023 performance year begins. Request a demo today to see for yourself how MatrixCare can prepare your agency to compete on value and succeed under HHVBP.
Request a demo today for a closer look at MatrixCare.
See what MatrixCare can do for you
Brandy Shifteh
Brandy Shifteh, RN, BHSA, MBA, joined MatrixCare in April of 2018 as a Clinical Informatics Business Analyst, where she has been very involved in the development and enhancement of clinical analytics that supports scrubbing of OASIS assessment data, casemix/HIPPS scoring, clinical assessment reviews and coding. In April of 2019, she transitioned into a Regulations Compliance role, where she is responsible for monitoring regulations that impact home health, hospice and private duty home care, to help ensure our solutions support all existing and new regulations. She is very plugged into the regulatory community with relationships at both the state and federal level and serves as an active member on the National Government Services (NGS) Vendor Coalition group, where she provides input on MAC provider education and materials. Brandy is a Registered Nurse and comes to us with over 23 years of operations management experience in the home health, hospice and private duty home care sector, inclusive of accreditation/survey preparedness, compliance and clinical/quality improvement programming. She holds two undergraduate degrees; science and nursing and health services administration; and an MBA in computer information systems (CIS).
Related Posts



See MatrixCare in action
Start by having a call with one of our experts to see our platform in action.
MatrixCare offers industry-leading software solutions. Thousands of facility-based and home-based care organizations trust us to help them improve efficiency and provide exceptional care.





